The bottom line is – that each disorder can make the other worse. Untreated mental health issues can be a hindrance to a person’s addiction recovery. Therefore, it is imperative to get treatment for both disorders.
Roughly 37% of alcohol abusers and 53% of drug abusers have at least one other serious mental illness.
Both addiction and mental health are complex conditions, underscoring the necessity for a profound comprehension of each before embarking on addiction treatment.
Comprehensive treatment, which delves into both the addiction and the co-occurring disorders, is crucial for the best chance at recovery. This article will provide a detailed exploration of co-occurring diagnoses, empowering you to understand and address them effectively.
What Is A Co-Occurring Disorder?
Co-occurring is the definition of two medical conditions simultaneously: chronic, acute, and long-term.
Addiction is associated with mental health disorders such as ADHD, Bipolar, Depression, anxiety, panic disorder, and more.
Multiple factors can contribute to the development of addiction and co-occurring disorders. The complexity of the disorder makes it difficult to quantify whether the mental health disorder or SUD (Substance Use Disorder) and AUD (Alcohol Use Disorder) came first.

Individuals with SUD or AUD may engage in the following behaviours;
- Cope with Mental Health issues through drug and alcohol abuse.
People who suffer from mental health issues will often turn to drugs or alcohol and “self-medicate” to alleviate the mental distress they are experiencing.
- Substance-induced mental health disorders
Abusing drugs or alcohol can induce mental health disorders, especially in individuals who are predisposed to them already.
- Develop Both Due To Risk Factors
Environmental and social factors, as well as trauma, can all lead to the development of substance use disorders as well as mental health issues.
How Common Are Co-Occurring Disorders?
Statistics reveal a distressingly high rate of comorbidity between mental health issues and substance abuse, underscoring the urgency of addressing co-occurring disorders. Here are some of the findings:
- It is estimated that 50% of individuals who have a substance use disorder will also experience a mental health disorder within their lifetime.
- It has been said that 30% of individuals with debilitating mental health issues will experience substance use disorders within their lifetime.
- In 2020, It was estimated that American adult individuals who have mental illness were more inclined to binge drink and chain smoke compared to those without a diagnosis.
- 43% of prescription medication abusers displayed symptoms of mental health issues or have been diagnosed with co-occurring mental health disorders.
- A study was done in 2020 and quantified that 17 million Americans over the age of 18 had an addiction and mental health disorders.
- In 2020, a study was conducted, and the results concluded that American adults were twice as likely to abuse drugs and alcohol than were previously diagnosed with a mental health disorder.
Signs of Co-Occurring Disorders
Only a licensed medical professional can diagnose a co-occurring disorder. This is crucial to ensure accuracy and an in-depth understanding of the illnesses. These professionals use a set of criteria outlined in the DSM-5, a manual used to diagnose mental health disorders, to diagnose substance use disorders.
Below are common mental health issues that co-occur with substance abuse;
- Panic Disorder – Frequent spells of hot flushing, dizziness, chills, heart palpitations, and hyper-ventilation characterise panic attacks. People with panic disorders report feeling like they are losing control and dying.
- Depression – Depression is often reported as severe feelings of hopelessness, deep sadness, loss of interest in once enjoyable activities, and lingering anhedonia.
- Generalised Anxiety Disorder (GAD) – GAD is characterised by an abnormal reaction with worry to frequent events that occur in everyday life; these include work, relationships, finances, and more.
- Agoraphobia – People who suffer from this disorder are intensely afraid of being stuck in places where they would not have a chance to escape.
- Social Anxiety Disorder – People who experience this disorder are debilitated by the fear of being humiliated or embarrassed in public; this impacts an individual’s ability to perform in social situations.
- Antisocial Personality Disorder (ASPD) – Common traits that are associated with ASPD include impulsivity, irritability, aggressiveness, and lack of remorse.
- Schizophrenia – Schizophrenia is characterised by the following symptoms: hallucinations, disorganised speech, delusions, mania, poor hygiene, and slowed speech.
- Borderline Personality Disorder – People who experience BPD suffer from fluctuations between episodes of depression and mania. The emotional dysregulation that is associated with this disorder makes it difficult for a person to manage their mental state.
- Anorexia Nervosa – Individuals who suffer from this disorder restrict their food intake and over-exercise out of fear of gaining weight.
- Bulimia Nervosa – People with Bulimia consume excessive amounts of food in a short time with feelings of losing control; this is followed by self-induced vomiting or misuse of laxatives.
- Binge Eating Disorder – Binge Eating involves consuming large quantities of food while feeling the inability to stop.
- ADHD – People with ADHD experience symptoms of the following: hyperactivity, inattentiveness, excessive talking, irritability, difficulty concentrating, and fidgeting.
- PTSD – A person who has PTSD may experience intrusive re-occurring thoughts of a traumatic event, which can feel like it is being experienced all over again. Feelings of irritability, social withdrawal, tiredness, etc, characterise PTSD.

How to Treat a Co-Occurring Disorder
When a person gets admitted into treatment, they will undergo an assessment and evaluate three pertinent things that can influence their stay;
- The severity of their substance use disorder and how long they have been active.
- Their home and social situation and the level of influence it has on them.
- An evaluation of their physical and mental health.
If a mental health screening is conducted and a co-occurring disorder is diagnosed, a more thorough test will be performed to examine the issue at hand; once that is done, a treatment plan will be developed and tailored to the patient’s specific needs. Individualised treatment is beneficial, as patients can achieve maximum clinical and inpatient treatment results.
Individuals are constantly monitored throughout their stay in rehab treatment; as their needs change, so does their inpatient program. Once cleared of substances, mental and physical health will gradually improve. This means that the intensity of the rehab treatment program, i.e., treatment duration, medical detox, etc., may change throughout a person’s stay.
Integrated care in rehab treatment centres is the optimal approach when dealing with co-occurring disorders. This approach combines treatments for both substance use disorders and mental health disorders, prioritising dual recovery goals. It often involves a team of professionals working together to provide comprehensive care, including psychiatrists, therapists, and addiction counsellors.
Our Co-Occurring Disorder Treatment in Johannesburg
Changes Addiction Rehab in Johannesburg is a rehab treatment facility equipped to treat drug and alcohol abuse. Our services include specialised clinical treatment, reintegration, and family support. Our treatment centre prioritises your loved one’s well-being by delivering individualised programs catering to their needs. The clinical team at Changes is committed to treating and improving the lives of our patients.
Our facility has a holistic therapeutic approach focusing more on just the impact addiction has had on an individual, treating the mental, physical, spiritual, and social domains.
We are a fully equipped three-phase rehab with primary, secondary, and tertiary care facilities.
Our clinical team includes:
- Psychologists
- Psychiatrists
- Occupational Therapists
- Medical Doctors
- Nurses
- Registered Counsellors
- Social Workers
- Halfway House Managers
- Recovery Assistants
Therapeutic approaches used at Changes:
- Cognitive Behavioral Therapy (CBT)
- BrainWorking Recursive Therapy
- Motivation Enhancement Therapy
- 12 Step Recovery
- Group Therapy
- Individual Counselling
- Occupational Therapy
- Addiction & Recovery Lectures
Substance use disorders are complex, and when they are present with another disorder, it can make them more complicated to treat, which is why an integrated therapeutic approach is the best way to treat it.
Addiction and mental health disorders are not death sentences, and if they are treated appropriately, individuals can function within society and live a life filled with happiness and joy.
Can someone have more than one substance use disorder?
Yes, an individual can have more than one, such as alcohol abuse disorder and opioid abuse disorder.
What is the most common co-occurring disorder?
General Anxiety Disorder (GAD) – This disorder is also most associated with self-medicating behaviours.
How can I prevent my risk for a co-occurring disorder?
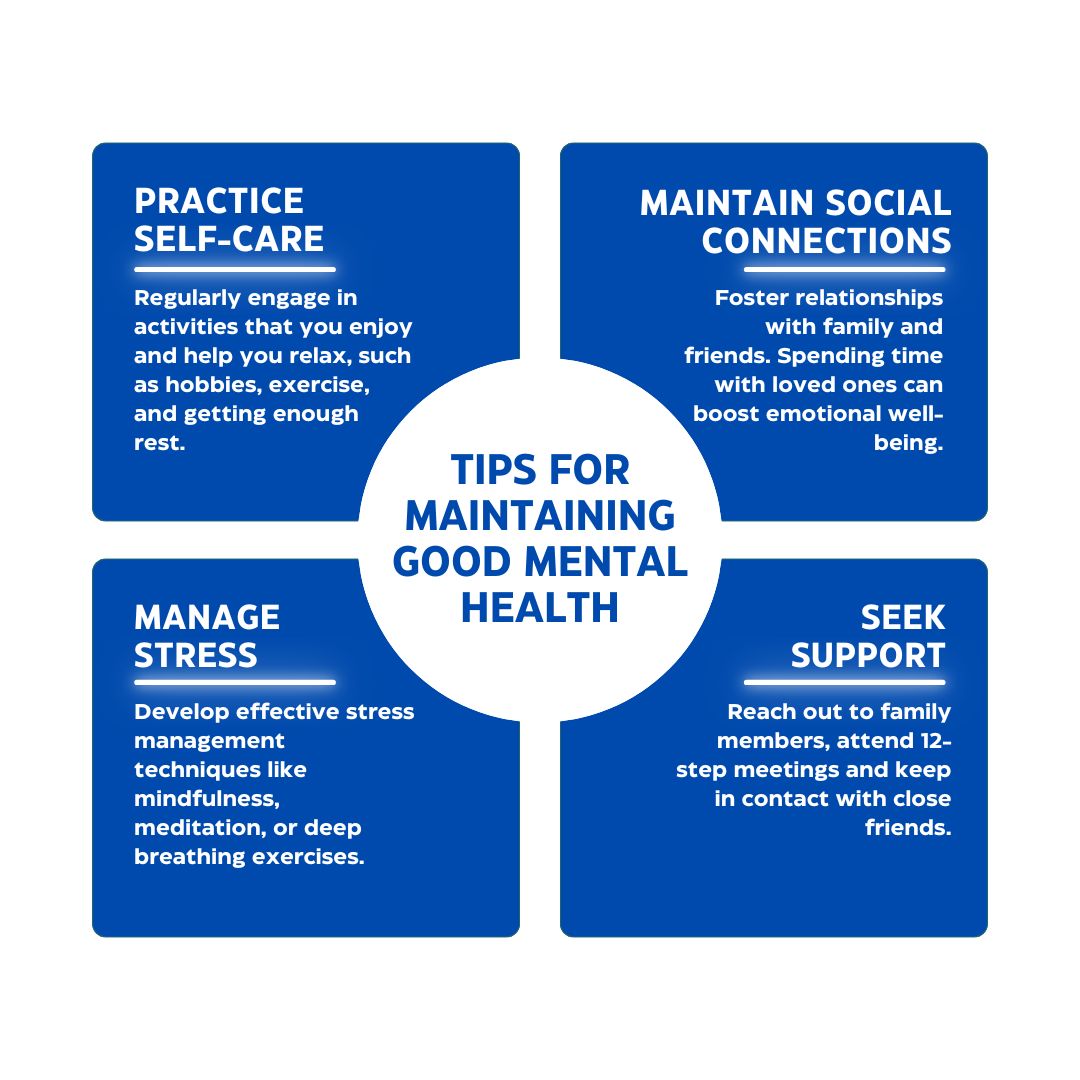
Mental health and substance use disorders are both brain diseases, which means they cannot be cured. However, they can be managed by the following:
- Being proactive by learning about your pre-dispositions.
- Looking after your physical health.
- Looking after your mental health, e.g., seeing a therapist.






