Does your medical scheme cover up to 21 days of inpatient rehabilitation and a medically supervised detox for addiction?
Medical Aid Covers Up To 21 Days Of Inpatient Rehabilitation
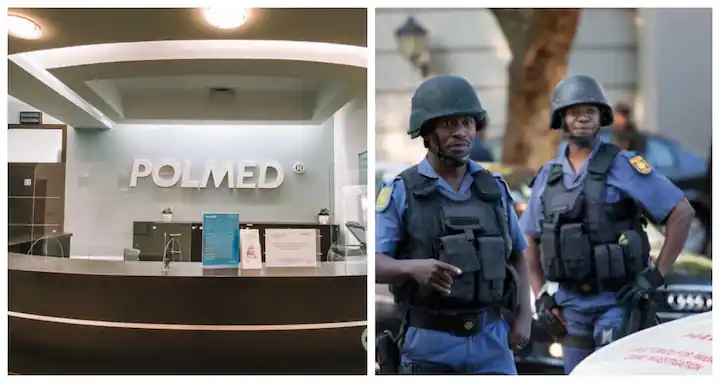
 Working in SAPS (South African Police Service) is incredibly stressful, and this opens SAPS members to the risk of developing addictions. The South African Police Service Medical Scheme (POLMED) understands the challenges faced by its members and does cover rehabilitation centre treatment for addictions.
Working in SAPS (South African Police Service) is incredibly stressful, and this opens SAPS members to the risk of developing addictions. The South African Police Service Medical Scheme (POLMED) understands the challenges faced by its members and does cover rehabilitation centre treatment for addictions.
POLMED Medical Aid Coverage Overview
Polmed aims to provide comprehensive care for its SAPS members. Here’s what you might find regarding addiction treatment:
- Prescribed Minimum Benefits (PMBs): As with other medical aids, addiction treatment is covered under PMBs. This includes inpatient rehab and detoxification services.
- Focused Treatment Programs: POLMED might have specific programs or dedicated care pathways for addiction and mental health treatment.
- Inpatient Coverage: POLMED covers a substantial portion of costs associated with inpatient rehabilitation at approved facilities for each policy member. Yes, this includes spouses and children.
- Outpatient Support: Some plans include coverage for outpatient therapy, support group participation, and medication management post-rehab.
- Limits and Co-payments: Addiction treatment has annual limits, and you may have to pay co-payments, even if it is covered.
Network of Providers
POLMED works with a network of accredited treatment centres and mental health professionals. Contact us today at 081-444-7000 to find providers specializing in addiction treatment that POLMED covers.
Getting Treatment Authorised
- Approval Process: You’ll need pre-authorization for addiction treatment. Call us today, and we’ll contact POLMED with the relevant ICD-10 codes for your pre-auth. You do not need to go through your doctor or a specialist to demonstrate medical necessity.
- POLMED’s Role: POLMED’s call centre will liaise with us and clarify exactly what they’ll cover, leaving you with a precise figure for your co-payment for the right treatment option.
Important Considerations
- Specific Benefits: If your POLMED policy has been running for more than a year, and is up-to-date, they’ll probably confirm 21 days of inpatient rehabilitation treatment for you or your loved one on the policy.
- Policy Updates: You’ll need to provide us with your up-to-date POLMED medical aid details, as medical aid policies may change.
- POLMED Medical Aid
- Understanding POLMED Medical Aid and Rehabilitation Coverage
- Overview of Polmed’s Health Services
- Polmed’s Health Insurance Plans
- Comprehensive Coverage Overview
- Specifics of Rehabilitation Services Coverage
- Rehabilitation Centres and Services Covered by Polmed
- Types of Rehabilitation Services
- Conditions and Treatments Covered

- Navigating Polmed Coverage for Rehabilitation
- Eligibility Criteria for Coverage
- Process for Claiming Rehabilitation Services
- Limitations and Exclusions of Polmed’s Rehabilitation Coverage
- What Polmed Does Not Cover
- Understanding the Fine Print
- Comparing Polmed with Other Health Insurances on Rehabilitation Coverage
- Competitive Analysis
- Choosing the Right Plan for Your Needs
- Member Experiences with Rehabilitation Services Through Polmed
- Success Stories
- Areas for Improvement
- Expert Tips for Maximizing Rehabilitation Coverage with Polmed
- Strategies for Claiming Benefits
- Avoiding Common Pitfalls
- The Future of Rehabilitation Coverage Medical Aid
- Trends and Predictions
- How Polmed is Adapting
- Conclusion
- Summary of Key Points
- Final Thoughts on Navigating Polmed Coverage for Rehabilitation
- FAQs
- Common Questions About Polmed and Rehabilitation Centres
Does Polmed Cover Rehabilitation Centres?
Trying to ascertain whether POLMED will cover a rehabilitation centre can seem overwhelming. Polmed offers various plans that cover rehabilitation centres because addiction to alcohol or other drugs is a PMB (Prescribed minimum benefit). We’ll help you understand Polmed’s coverage for rehabilitation centres, ensuring that you have all the information you need to access the services you or your loved ones may require.
 Polmed’s Medical Aid Plans
Polmed’s Medical Aid Plans
Polmed provides a range of health insurance plans designed to cater to different needs. These plans cover various healthcare services, from routine check-ups to specialized care, including addiction rehabilitation. Let’s look at how these plans address rehabilitation centres and what members can expect regarding medical aid coverage.
Rehabilitation Centres and Services Covered by Polmed
Rehabilitation treatment is crucial for individuals hoping to recover from addiction to alcohol and/or drugs. Addiction is a chronic condition, and Polmed medical aid is required by law to recognise this as a PMB (Prescribed minimum benefit). POLMED, therefore, covers rehabilitation centres under its medical aid plans.
Navigating Polmed Coverage for Rehabilitation
Understanding the eligibility criteria and the claiming process is critical to accessing rehabilitation services through Polmed. Call us today at 081-444-7000 for a quick pre-authorisation. It’s a brief call to Polmed with all the right data, and we’ll know within minutes what your Polmed medical aid plan will cover.
 Does Polmed Cover Rehabilitation Centres
Does Polmed Cover Rehabilitation Centres
No insurance coverage is without its limitations and exclusions. Members need to be aware that if they’ve just joined Polmed medical aid or if their policy is not up-to-date, it’s unlikely that Polmed will pay for treatment at an addiction rehabilitation centre. This will help them set realistic expectations and plan accordingly.
Comparing Polmed with Other Health Insurances on Rehabilitation Coverage
Choosing the right health insurance is a critical decision. As addiction treatment is a legal PMB in South Africa, all Polmed plans cover rehabilitation. This is true of hospital plans and medical aids throughout South Africa.
Member Experiences with Rehabilitation Services Through Polmed
Changes Addiction Rehab has at least 8 to 10 SAPS members through our Primary Care rehab centre monthly. We have real experience dealing with South African Police and the trauma they’ve suffered. Being a police officer in South Africa is unlike anywhere else and comes with very specific difficulties. Often, SAPS members are concerned that their careers will be affected if they attend a drug and alcohol rehabilitation centre.
Polmed medical aid members are given a sick note for their time away from work that does not divulge why they were off. We do all we can to return out SAPS members back to full functioning at work and want their careers to flourish. We would not want a faultless brain disease to hinder their working life. We have many positive outcomes and return patients to better functioning at home and work.
 Expert Tips for Maximizing Rehabilitation Coverage with Polmed
Expert Tips for Maximizing Rehabilitation Coverage with Polmed
Maximizing your addiction rehabilitation coverage is easy. Let us handle the pre-authorisation details on your behalf. Our expert admin staff spend a large proportion of their time on the phone with medical aids, giving the correct data to ensure that members can get help.
Call us today at 081-444-7000
If You Need More Information About Medical Aid Coverage For Addiction Treatment Click On The Following Links:
- LA Health
- Remedi
- Bestmed
- Medscheme
- Momentum
- Discovery
- Multi-Choice
- Compcare
- Genesis
- Medshield
- Gems
- Fedhealth
- SABC
FAQ: Polmed Medical Aid Rehab Cover
Does Polmed cover inpatient rehabilitation and detox?
Yes. Polmed provides cover for inpatient substance abuse rehab under its hospital/mental health benefits, subject to scheme rules, medical necessity, and authorisation.
How many days of rehab does Polmed fund per year?
Polmed typically allows up to 21 days of inpatient rehabilitation (including detox), but this may vary based on your specific plan.
Are outpatient or aftercare services covered by Polmed?
Outpatient services such as counselling, therapy or outpatient detox are generally excluded unless your plan explicitly includes them beyond PMB entitlements.
What does Polmed require for pre-authorisation?
Pre-authorisation is mandatory. You must submit the patient’s medical aid details, ID, ICD-10 codes and practice numbers, and wait for scheme approval before admission.






